Sickle cell disease is the most common inherited blood disorder in the United States. Children with sickle cell disease experience episodes of severe pain and ongoing medical challenges. Early and ongoing medical care and treatment can minimize complications and help children with the disorder lead full and active lives.
Learn about promising treatments approved for people with certain types of sickle cell disease here.
How does sickle cell disease affect children?
In children with sickle cell disease, a protein called hemoglobin that carries oxygen inside the red blood cells forms chains that clump together and cause the red blood cell to be shaped like a crescent moon or the letter C―called a sickle cell.
Compared to normal red blood cells that are disk-shaped and flexible, sickled cells are stiff, sticky and fragile. They break apart and leave the blood stream sooner than normal red blood cells. This results in blocking of normal blood flow, preventing blood, and the oxygen it carries, to get to everywhere in the body.

Image Source: U.S. National Library of Medicine
How do infants and children get sickle cell disease?
Babies are born with sickle cell disease. Sickle cell disease is a genetic condition, so children get it in the same way they inherit the
color of their eyes, skin, and hair through the combination of genes they inherit from their parents.
How is sickle cell disease inherited?
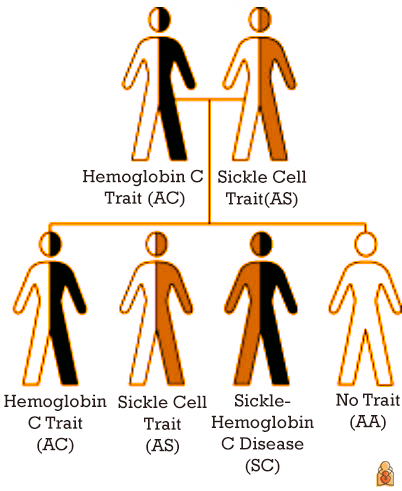 Everyone inherits one hemoglobin gene from their mother and one hemoglobin gene from their father. Inheriting one mutated or abnormal gene, but having a normal gene from the other parent, is called having a trait. Inheriting two abnormal hemoglobin traits or genes determines whether a child has sickle cell disease.
Everyone inherits one hemoglobin gene from their mother and one hemoglobin gene from their father. Inheriting one mutated or abnormal gene, but having a normal gene from the other parent, is called having a trait. Inheriting two abnormal hemoglobin traits or genes determines whether a child has sickle cell disease.
The normal hemoglobin gene is labeled A. The most common mutated hemoglobin genes or hemoglobin traits are called S or C. The mutated (changed) hemoglobin gene associated with sickle cell disease is S. Common types of mutated (changed or abnormal) hemoglobin genes that combine with S to cause sickle cell disease are S, C and beta thalassemia.
People who have inherited one of the following gene combinations
DO NOT have sickle cell disease:
A + A (AA): no sickle cell disease
A + S (AS): carrier of the hemoglobin "S" gene, known as sickle cell trait
A + C (AC): carrier of the hemoglobin "C" gene
People who have inherited one of the following gene combinations DO
have sickle cell disease:
S + S (SS):
Sickle cell anemia or Hemoglobin SS
S + C (SC):
Sickle hemoglobin C disease or Hemoglobin SC
S + beta thalassemia trait (S-beta thalassemia): a form of sickle cell disease
Image source: Centers for Disease Control and Prevention
How do I know if my baby has sickle cell trait or disease?
Every state in the U.S. performs a
newborn screening test for sickle cell disease. If this test is concerning for sickle cell disease, the baby is referred to a pediatric hematologist. If the test indicates
sickle cell trait, the parents are counselled by their pediatrician and the child generally does not need to see a hematology specialist.
Early diagnosis—before infants show any symptoms—allows infants with sickle cell disease to get early treatment and can help lower their risk of infections and other serious problems.
Why is sickle cell disease more common in children of African heritage?
A carrier of a single hemoglobin S gene is said to have sickle cell trait or hemoglobin S trait. About
1 in 12 people of African ancestry carry S trait. Sickle cell trait is also common in people with ancestors from the Caribbean, Middle East, India, South America, Central America and Mediterranean countries such as Turkey, Greece and Italy. Sickle cell trait is found today in descendants of these populations no matter where they live.
People with hemoglobin S trait alone do not have sickle cell disease. However, if their reproductive partner also has the hemoglobin S trait, then together they have a 1 in 4 chance (25%) of having a child with sickle cell disease. This is why
biracial and multiracial children can have sickle cell disease; About
1 in 365 Black or African American people are born with sickle cell disease each year in the United States.
Why is sickle cell disease sometimes called sickle cell anemia?
Sickle cell disease is an umbrella term for the many specific types of sickle cell disorders.
Anemia―meaning a lower-than-normal hemoglobin in red blood cells―happens with all forms of sickle cell disease. While normal red blood cells can live for 120 days, sickled cells last only 7 to 20 days; the body can't replace them fast enough resulting in anemia.
Children who have inherited two abnormal genes have sickle cell disease; which specific genes have been inherited determines what the disorder is called. Sickle cell anemia refers to the two most severe forms of sickle cell disease, hemoglobin SS and sickle beta zero thalassemia.
Main Types of Sickle Cell Disorders |
Hemoglobin SS | The most severe form, affecting 65% of children with sickle cell disease. Most or all of the hemoglobin is abnormal, causing chronic anemia. |
Hemoglobin SC disease | Roughly 25% of children with sickle cell disease have this mild to moderate form of the disease. Symptoms generally develop later in childhood, but may be as severe as in SS. |
Sickle beta plus thalassemia | Affects around 8% of children with sickle cell disease. This is generally considered a mild form of sickle cell disease, but severity can vary greatly. |
Sickle beta zero thalassemia | A severe but less common form, accounting for 2% of sickle cell disease. It is similar to hemoglobin SS.
|
Why are infants and children with sickle cell disease at higher risk of infection?
Sickle cell disease may cause damage to the spleen, kidneys, lungs and brain. Once damaged by sickled cells the spleen may not be able to filter bacteria from the blood as well as normal.
As a result, infants and children with sickle cell disease have a compromised immune system, which means they are more likely to have certain infections which may be fatal.
Antibiotics to prevent secondary infections in infants & children with sickle cell disease:
National guidelines recommend newborns diagnosed with severe sickle cell disease (SS and S beta zero thalassemia) receive antibiotics twice a day until they are 5 years old.
Research shows that children with sickle cell anemia given twice daily penicillin (an antibiotic) had 84% less risk of Streptococcus pneumoniae bacterial infection, which can cause serious conditions like pneumonia and meningitis.
Is there a treatment or cure for sickle cell disease?
Sickle cell disease is a chronic disease. Until recently, there were very few treatment options. Early diagnosis and starting antibiotics shortly after birth for those with severe forms of sickle cell have greatly improved life expectancy.
There are a few options available now to prevent serious problems, depending on the type of sickle cell disorder. They include
hydroxyurea (for age 2 years and older),
L-glutamine (for age 5 years and older),
voxeltor (for age 4 years and older) and
crizanlizumab (for age 16 years and older).
Bone marrow/stem cell transplant. This treatment can cure sickle cell disease. It is a procedure that takes healthy cells that form blood from a donor with suitable bone marrow. The bone marrow must be a close match that usually comes from a brother or sister. Only approximately 25% of patients have a matched sibling as a donor for this option.
Cell-based gene therapies. The Food and Drug Administration (FDA) approved
new therapies (exa-cel and lovo-cel) to treat sickle cell disease in people age 12 years and older—especially those who often have serious problems from sickle cell that lead to hospitalization. Both therapies use the patients' own blood stem cells. Their cells are collected and modified. Then, the patient receives a chemotherapy drug to remove cells from their bone marrow. The patients' modified stem cells are given back to them to produce hemoglobin that prevents sticking of the red blood cell. Learn more about sickle cell disease gene therapy from the
National Human Genome Research Institute.
Who are the doctors that care for children with sickle cell disease?
In addition to regular visits with their pediatrician, children with sickle cell disease should see a
pediatric hematologist at least periodically. These doctors specialize in the care of children with sickle cell disease.
More information: