By: Anthony Porto, MD, MPH, FAAP
It can be difficult to know whether your infant or child is having symptoms of lactose intolerance or whether he or she may have a milk allergy.
The following frequently asked questions from parents will help you learn more about the common symptoms of lactose intolerance, diagnosis, and treatment options.
Is lactose intolerance the same thing as a milk allergy?
No. Many parents confuse the terms lactose intolerance and milk allergy. While they may share similar symptoms, they are entirely different conditions. Lactose intolerance is a digestive problem, while milk allergy involves the immune system. So, while lactose intolerance can cause a great deal of discomfort, it will not produce a life-threatening reaction such as anaphylaxis.
Milk allergies tend to appear within the first year of life, while an infant's digestive system is still quite immature. Lactose intolerance can start in childhood into adolescence and can become more noticeable into adulthood.
What is lactose?
Lactose is a sugar found in foods that many children love—milk and dairy products, such as frozen yogurt and cheeses. The list of other foods containing lactose is long and includes some breads, cereals, and frozen or canned foods.
Lactose is broken down by the lactase enzyme located in the small intestine—the organ where most food digestion and nutrient absorption takes place. When we eat lactose, lactase breaks lactose down into two simple sugars: glucose and galactose. The body then absorbs these simple sugars into our intestines. When there is a decrease or loss of the lactase enzyme, we cannot break down or absorb lactose. The unabsorbed lactose can lead to symptoms, which is called an intolerance.
In addition to milk, what other food products contain lactose?
Lactose is present in many food products and in some medications. Manufacturers also often add milk and milk products to boxed, canned, frozen, packaged, and prepared foods. People who have digestive symptoms after consuming a small quantity of lactose should be aware of the many food products that may contain even small amounts of lactose.
You can check the ingredients on food labels and the nutrition facts to find possible sources of lactose in food products. If a food label includes any of the following words, the product contains lactose:
Milk
Lactose
Whey
Curds
Milk by-products
Dry milk solids
Nonfat dry milk powder
What are some key symptoms of lactose intolerance?
The symptoms of lactose intolerance depend on the amount of lactose that's consumed. The more lactose your child consumes, the more symptoms he or she will experience. Symptoms of lactose intolerance can occur within minutes to hours after drinking milk or eating dairy products and range from mild to severe based on the amount consumed and the amount tolerated. Here are symptoms you should look out for:
If I think my child might be lactose intolerant. How can I tell?
One way to check if your child has trouble digesting lactose is to take all the milk products out of your child's diet for two weeks and to then see if his or her symptoms improve. After two weeks, slowly reintroduce the products in small amounts each day to see if symptoms return. Your pediatrician can also test your child for lactose intolerance with a hydrogen breath test.
I've heard lactose intolerance can sometimes be a temporary side effect when kids are sick. Is that true?
Yes. Lactose intolerance can occur temporarily in children after a viral infection (that is why you may be told to avoid milk with lactose in it during a stomach bug) or it may be seen with conditions that lead to inflammation of the intestines, such as celiac disease.
Can infants be lactose intolerant?
Lactose intolerance is actually not very common in infants and typically only starts showing up after age three in children who were born full-term. All babies are born with lactase in their intestines. As they grow older, the lactase enzyme decreases.
Babies who were born premature are more likely to have a type of lactose intolerance called developmental lactase deficiency. This condition usually lasts only for a short time after birth. However, the majority of premature infants will be able to consume lactose-containing formula and breast milk.
Congenital lactase deficiency is a very rare disorder in which babies can't break down the lactose in breast milk or formula. Genes inherited from parents cause this disorder. This type of intolerance results in severe diarrhea, and if not fed a lactose-free infant formula, those babies could develop severe dehydration and weight loss.
If a mother is lactose intolerant, is it safe for her to breastfeed her baby?
It's perfectly safe to breastfeed your child if you're lactose intolerant. Breastfeeding does not put your baby at greater risk of becoming lactose intolerant, and it has important health benefits for your baby.
How can my child get enough calcium in her diet if milk or lactose are reduced?
If your child has lactose intolerance, he or she can still eat lactose-free dairy products including lactose-free milk, cheese, and yogurts—all are good sources of calcium. In addition, your child can get calcium from dark green leafy vegetables such as spinach, broccoli and kale, nuts (almonds), beans (white beans), fish (sardines, salmon) and calcium-fortified orange juice. If you feel your child is not getting enough calcium, talk with your pediatrician about starting a calcium supplement.
Are soy or almond milks adequate substitutes for children who are lactose intolerant?
There are many milk substitutes that a child with lactose intolerance can drink, including soy, almond, rice, hemp, and oat milk. Soy milk is a popular milk alternative, because it is a good source of calcium and protein. Almond milk has also become a popular alternative and is safe for children with lactose intolerance or a cow's milk protein allergy. Although almond is a good source of calcium, it is lower in protein and contains fewer calories than cow's milk. Before starting any alternative milks, it is important to talk with your pediatrician about which may be best for your child.
How is lactose intolerance diagnosed?
Your pediatrician will take a medical, family, and diet history to help diagnose lactose intolerance in your infant or child. During this discussion, he or she will review your child's symptoms with you.
In some cases, a hydrogen breath test is done to test for lactose intolerance. For the test, your child breathes into a container that measures breath hydrogen level before and after he or she drinks a beverage that contains a known amount of lactose. Normally, only a small amount of hydrogen is detectable in the breath when a person eats or drinks and digests lactose. An increase in hydrogen levels is considered a positive test for lactose intolerance.
Pediatricians check acidity in the stools of infants and young children who may be unable to properly do the hydrogen breath test. Acidic stool (low pH) may indicate lactose malabsorption. Another stool test (reducing substances) looks for the presence of glucose in the stool, which signifies undigested lactose.
If your child's symptoms persist, he or she may be referred to a pediatric gastroenterologist (GI) for further evaluation. Depending on the severity of your child's symptoms, the GI may perform an endoscopy to measure lactase levels directly from the intestine. This is done with a biopsy.
How much calcium and vitamin D are recommended for my child to eat each day?
The specific amount is based on your child's age. Here is a breakdown of the Recommended Dietary Allowances (RDA) for calcium and vitamin D.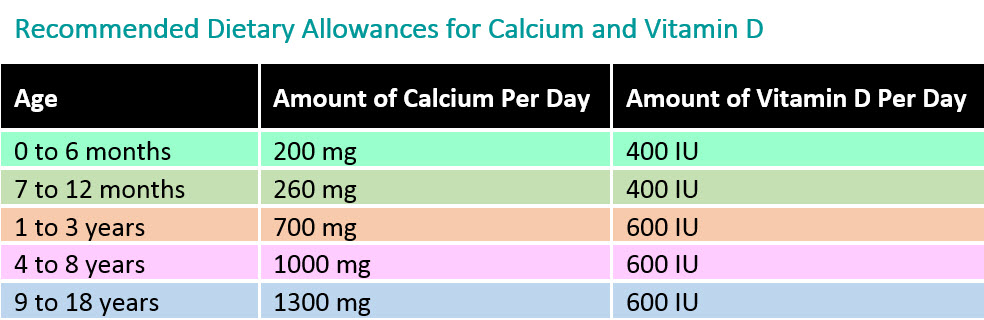
How is lactose intolerance treated?
How lactose intolerance is treated depends on the extent of your child's symptoms. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.
To help alleviate symptoms if/when your child consumes lactose-containing food, your pediatrician may recommend an over-the-counter lactase enzyme supplement.
If your child's symptoms are severe and warrant removing all lactose from his or her diet, your pediatrician may refer your child to a registered dietitian. Since dairy is a good source of calcium and vitamin D—which all kids need—a registered dietitian can suggest other foods to provide those nutrients and may suggest vitamin supplements.
Is lactose intolerance a lifelong condition?
In some cases, lactose intolerance is temporary—if lactose intolerance develops after a viral illness or if it is associated with other conditions, like celiac disease. For example, once celiac disease is treated, lactase levels can become in the normal range and lactose may be tolerated in the diet. More than likely, however, lactose intolerance is long-term and requires many older children and adults to alter their diet to avoid symptoms.
Additional Information & Resources:
About Dr. Porto:
 Anthony Porto, MD, MPH, FAAP is a board certified pediatrician and board certified pediatric gastroenterologist. He is an Associate Professor of Pediatrics and Associate Clinical Chief of Pediatric Gastroenterology at Yale University and Director, Pediatric Gastroenterology at Greenwich Hospital in Greenwich, CT. He is also the medical director of the Yale Pediatric Celiac Program. Within the American Academy of Pediatrics, Dr. Porto sits on the PREP Gastroenterology Advisory Board and is a member of the Section on Gastroenterology, Hepatology and Nutrition. He is also a member of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition's Public Education Committee, a pediatric expert on nutrition for The Bump's Real Answers, and is the co-author of The Pediatrician's Guide to Feeding Babies and Toddlers. Follow him on Instagram @Pediatriciansguide.
Anthony Porto, MD, MPH, FAAP is a board certified pediatrician and board certified pediatric gastroenterologist. He is an Associate Professor of Pediatrics and Associate Clinical Chief of Pediatric Gastroenterology at Yale University and Director, Pediatric Gastroenterology at Greenwich Hospital in Greenwich, CT. He is also the medical director of the Yale Pediatric Celiac Program. Within the American Academy of Pediatrics, Dr. Porto sits on the PREP Gastroenterology Advisory Board and is a member of the Section on Gastroenterology, Hepatology and Nutrition. He is also a member of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition's Public Education Committee, a pediatric expert on nutrition for The Bump's Real Answers, and is the co-author of The Pediatrician's Guide to Feeding Babies and Toddlers. Follow him on Instagram @Pediatriciansguide.