By: Price T. Edwards, MD & Patrick Reeves, MD, FAAP
Functional abdominal pain disorders (FAPDs) are the most common condition seen by pediatric gastroenterologists (digestive system doctors). FAPDs affect one in four children across the world. The disorders may be chronic, with ongoing abdominal pain, or cause stomachaches that come and go.
FAPDs in children typically have no clear cause. They fall under a type of diagnosis called disorders of gut-brain interaction (DGBIs). Constant communication exists between our brain and the nerves, which may cause pain in our gastrointestinal tract (GI) and the rest of our body.
FAPDs do not develop over the course of one day. It can take months or even years for a disorder to develop. Continue reading to learn about the symptoms, diagnosis, and treatment for FAPDs in children.
Symptoms of functional abdominal pain disorders
Most children with FAPDs will have pain at or around the belly button. Other more concerning symptoms can occur with FAPDs may include:
Nausea/vomiting
Headaches
Dizziness
Tiredness
Dysphagia (difficulty swallowing) or odynophagia (painful swallowing)
gastrointestinal bleeding
Nighttime
diarrhea
Skin changes around the bottom
Involuntary weight loss
Deceleration of linear growth, a slowing down of gain in a child's height or length
Delayed puberty
Unexplained/recurrent fever
Arthritis or inflamed joints
If your child has abdominal pain accompanied by any of these symptoms, or if you have a family history of inflammatory bowel disease (IBD) such as ulcerative colitis or Crohns disease, celiac disease or peptic ulcer disease, contact their doctor. These signs will need further testing and you may be referred to a pediatric gastroenterologist.
What causes gut-brain interaction & functional abdominal pain disorders in children?
The cause of pain from FAPDs and DGBIs is unknown, but
research suggests it can be associated with:
Stressful events, like a move or family separation
Changes to the bacteria that live in the gut (gut
microbiome)
Dysregulated autonomic nervous system, which controls digestion and and other automatic body functions such as heart rate
Family history of DGBIs, which suggests that genetics could play a role.
Disordered movement of the GI tract, when normal rhythmic contractions that move food and waste through your digestive system become irregular
How are DGBIs & FAPDs diagnosed & treated?
Typically, FAPDs require diagnosis and treatment from a doctor, and many children may feel better within a few days to a few weeks.
DGBIs are diagnosed through the evaluation of your child's symptoms by their doctor. There are different conditions that share symptoms, and a diagnosis will vary between children. One child may benefit from further testing while another child may not. Each child is different, so evaluating your child's symptoms may be the best way for their doctor to reach a diagnosis. Talk to your pediatrician to better understand your child's health.
Treatments typically depend on your child's symptoms and the type of DGBI they have. DGBIs can add stress and negatively impact quality of life for patients. The goal of many treatments is to reduce and manage symptoms so patients can stay involved in life activities.
Treatments for DGBIs and FAPDs include:
Child psychology or cognitive behavioral therapy (CBT). Studies suggest that both in-person and virtual use of CBT can be effective in treating FAPDs. Hypnosis and biofeedback training can also be effective
treatments.
Finding dietary triggers. It may be helpful to keep a journal to track foods that cause pain and symptoms of FAPDs. Some patients with IBS may respond well to less
FODMAPs, or foods with high levels of poorly digested sugars. Consult your pediatrician about the low-FODMAP diet for your child.
Medications. Medication use will vary depending on which DGBI has been diagnosed. For functional abdominal pain related to intestinal spasm, antispasmodic medicines are frequently used. Peppermint oil has also been shown to have an antispasmodic effect. Some medication may be prescribed to prevent episodes of FAPDs.
One study found probiotics helpful for FAPDs and irritable bowel disease. There is ongoing research into additional medication to treat and prevent DGBIs.
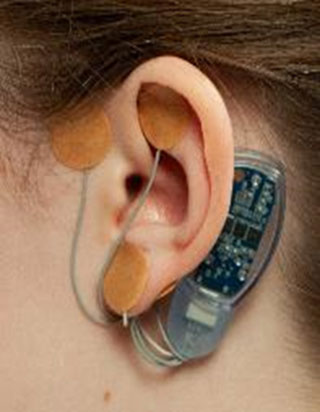
Acupunture & medical devices for FAPDs. Some treatments use auricular (ear/hearing) acupuncture with small needles. There are also devices being developed that use electrical stimulation that can treat FAPDs. Here are what the devices look like:

Remember
Reach out to your child's pediatrician if you have concerns about your child's gastrointestinal pain.
More Information
About Dr. Edwards
 Price T. Edwards is a pediatric gastroenterologist at Le Bonheur Children’s Hospital in Memphis, TN. His clinical focus is on neurogastroenterology and learning how to better diagnose and treat disorders of GI motility and pain. As a former teacher and current father of four, he values the importance of clear communication and lots of listening while at work and at home.
Price T. Edwards is a pediatric gastroenterologist at Le Bonheur Children’s Hospital in Memphis, TN. His clinical focus is on neurogastroenterology and learning how to better diagnose and treat disorders of GI motility and pain. As a former teacher and current father of four, he values the importance of clear communication and lots of listening while at work and at home. |
About Dr. Reeves
 Patrick T. Reeves, MD, FAAP, is a consultant Pediatric Gastroenterologist at Brooke Army Medical Center and a father of two. Dr. Reeves has published more than 20 PubMed cited articles, received three grant awards, developed two point-of-care medical applications, and created numerous clinical tools with the intent to improve patient care. He has a research focus is the development of medical education curricula and clinical point-of-care instruments to facilitate the care of children.
Patrick T. Reeves, MD, FAAP, is a consultant Pediatric Gastroenterologist at Brooke Army Medical Center and a father of two. Dr. Reeves has published more than 20 PubMed cited articles, received three grant awards, developed two point-of-care medical applications, and created numerous clinical tools with the intent to improve patient care. He has a research focus is the development of medical education curricula and clinical point-of-care instruments to facilitate the care of children.
Editor's note: Auricular neurostimulation device images courtesy Katja Kovacic, MD.
|